
The general, or desired goal of allopathic medicine (M.D.) is to obtain a cure. With chronic pain, that may be unrealistic. Given the biological, social, physical and psychologist contexts in which chronic pain may occur, it is probably more realistic to promote rehabilitation and to maximize quality of life (Mills, et. al. 2016).

Physicians generally recognize two types of pain (https://www.medicalnewstoday.com/articles/319895) :
- “Nociceptive pain is a medical term for pain from physical damage or potential damage to the body. Neuropathic pain refers to pain when an injury or medical condition damages the nervous system or prevents it from working properly. Examples of nociceptive pain include the pain felt from a sports injury, a dental procedure, or arthritis. Nociceptive pain is the most common type of pain people experience. It develops when the nociceptive nerve fibers are triggered by inflammation, chemicals, or physical events, such as stubbing a toe on a piece of furniture. Nociceptive pain is usually acute and develops in response to a specific situation. It tends to go away as the affected body part heals. For example, nociceptive pain due to a broken ankle gets better as the ankle heals. The body contains specialized nerve cells called nociceptors that detect noxious stimuli or things that could damage the body, such as extreme heat or cold, pressure, pinching, and chemicals. These warning signals are then passed along the nervous system to the brain, resulting in nociceptive pain. This happens very quickly in real time, which is why people know to remove their hands if they touch a hot oven or take the weight off an injured ankle. The information provided by nociceptive pain can help the body protect and heal itself.
- Neuropathic pain is a medical term used to describe the pain that develops when the nervous system is damaged or not working properly due to disease or injury. It is different from nociceptive pain because it does not develop in response to any specific circumstance or outside stimulus. In fact, individuals can suffer from neuropathic pain even when the aching or injured body part is not actually there. This condition is called phantom limb pain, which may occur in people after they have had an amputation.Neuropathic pain is also referred to as nerve pain and is usually chronic. Many different conditions and diseases cause neuropathic pain, including:
- diabetes
- multiple sclerosis
- stroke
- cancer
- cytomegalovirus
- amputation “
According to the Pain Center of Arizona (https://www.thepaincenter.com/blog/types-of-chronic-pain-syndromes/ ), chronic pain syndrome can develop due to several things, including:
Existing injury. Injuries can cause tissue damage, leading to chronic pain and prolonged healing.
Coexisting medical condition (including psychological such as depression or anxiety). Medical conditions like fibromyalgia, spinal stenosis, or arthritis significantly affect chronic pain. Mental health problems like depression, anxiety, and long-term stress can cause physical side effects like muscle spasms, contributing to chronic pain.
Post-surgery. Pain often lingers following surgery. Without proper physical therapy or treatment, chronic pain can develop.
Lifestyle. Habits of poor posture, sedentary living, and eating unhealthy foods contribute to physical problems like spine pain. Without addressing these issues, the pain can linger and progress.
Environmental factors. Poor air quality or exposure to chemicals and toxins can harm the body and bring about chronic pain problems.
Genetics. If certain conditions are inherited, such as fibromyalgia or sickle cell anemia, this can contribute to chronic pain, more so if the condition itself is not addressed.
Furthermore, the illnesses that are typically associated with high levels of pain include:
Cancer: Cancer pain may result from cancer itself (exerting pressure on organs) or from cancer treatment (i.e. chemotherapy, radiation therapy). Patients may find relief from cancer pain through interventional pain treatment.
Fibromyalgia: Fibromyalgia is a condition that may cause widespread musculoskeletal pain, fatigue, behavioral health, and cognitive health issues. Musculoskeletal pain typically affects the bones, muscles, ligaments, tendons, and nerves in the body and can worsen with movement, overuse, or sleep disturbances. Currently, there is no known cure for fibromyalgia.
Endometriosis: Endometriosis causes the uterus lining to grow outside of the uterus on other pelvic organs. This tissue thickens and bleeds, as typical endometrial tissue does during menstrual cycles. The misplaced tissue can cause intense pelvic pain, and women with chronic pelvic pain may experience heavy periods or infertility.
Endometriosis can impact the ovaries can cause endometriomas cysts to form. The cysts can irritate surrounding tissue and develop scar tissue and adhesions, making pelvic tissue and organs attach together.
Multiple sclerosis (MS): Multiple sclerosis (MS) is a chronic disease that affects the central nervous system (brain, spinal cords, and optic nerves). With MS, the immune system attacks itself, destroying the protective covering of nerves. This leads to painful and debilitating symptoms that vary depending on the severity of the disease.
Complex regional pain syndrome (CRPS): Complex regional pain syndrome (CRPS), formerly known as reflex sympathetic dystrophy (RSD), is a chronic, painful condition affecting the arms or legs.
Symptoms typically include severe chronic pain, inflammation, and changes in skin color and skin temperature.
Rheumatoid arthritis: Rheumatoid arthritis is a chronic, autoimmune disorder that causes inflammation to smaller joints in the hands and feet. This particular form of arthritis affects the lining of joints, which can result in bone erosion and joint deformity overtime.
Chronic migraines: Migraines cause throbbing or pulsating pain in one area of the head, followed by fatigue and irritability. Severe cases of migraine can be debilitating and cause diarrhea, nausea, or auditory and visual distortions. Migraine attacks may last anywhere from a few hours to a few days, and could be preceded or accompanied by visual disturbances known as auras.
Modalities of treatment
There are 3 main modalities of treatment, which will be discussed here: Pharmacological, surgical, and complementary
I. Pharmacological
Pain is frequently reported during cancer disease, and it still remains poorly controlled in both patients currently being treated and in patients who have successfully completed their rounds of chemotherapy, i.e. cancer survivors (Mestdagh, et. al., 2023). For cancer patients at least, pain management has relied on pharmacotherapy, with opioids being considered the mainstay, despite their common side effect including nausea and vomiting, constipation, sedation, dizziness, hallucinations, and respiratory depression, tolerance and dependence. The recent opioid epidemic has prompted practitioners to reassess the use opioids in the treatment of cancer pain, favoring an integrative approach, which would include analgesics and adjuvants, (adapted from Table 1 in Mestdagh, et. al., 2023).
| Analgesics | |||
| Nonopioid | Paracetomal, NSAID’s | Every patient, if indicated | |
| Weak opioids | codeine, hydrocodone, tramadol | Mild-to-moderate pain in association with nonopioid: Tramadol: second line for neuropathic pain | |
| Strong opioids | – First line: Morphine, oxycodone, hydromor-phone –Second line: Methadone, buprenorphine, tapentadol | Moderate to severe pain | |
| Adjuvants | |||
| Ketamine | Refractory chronic pain | ||
| Magnesium | Hypomagnese-mia, refractory cancer pain | ||
| Tricyclic antidepressants (TCA) | Amitriptyline, nortriptyline | Neuropathic pain | |
| Serotonin and norepinephrine reuptake inhibitors (SNRI) | Duloxetine, vanlafaxine | Neuropathic pain | |
| Anticonvulsant | Gabapentin, pregabalin | Neuropathic pain | |
| Cannabis-related medicines | Chronic pain | ||
| Lidocaine infusion | Refractory neuropathic pain, refractory visceral pain | ||
| Topical treatment | Lidocaine, capsaicin | Localized neuropathic pain |
II. Surgical
The Pain Center of Arizona (https://www.thepaincenter.com/blog/types-of-chronic-pain-syndromes/) offers the following FDA-approved and minimally invasive surgical procedures to reduce pain with minimum downtime and discomfort.
The Pain Center offers unique treatments for chronic pain that are FDA-approved and minimally invasive procedures that reduce pain with minimal downtime and discomfort.
Their treatments include:
TPC Spine Stim
TPC Spine Stim is for patients with chronic back or leg pain who haven’t responded to alternative, conservative treatments in the past six months. The TPC Spine Stim works by implanting a nerve stimulation device into your spine. This device delivers low-voltage electrical currents to areas of the spine to reduce the pain signals causing chronic pain.
TPC Spine Fuse
TPC Spine Fuse targets spinal degeneration, usually brought on by stenosis, spondylolisthesis, and related conditions. It works to alleviate pain due to pressure on the spinal cord and instability that causes painful movements of the vertebrate.
In this procedure, a small incision goes into the back under live X-ray guidance. A device is placed between the spinous processes that fuse the segment. This gives the back stability, where the bones shift forward and backward. Our procedure can also be done through alternative approaches (a posterior, oblique, or lateral approach) depending on each individual’s needs.
TPC Spine Lift
TPC Spine Lift is a spinal decompression treatment aiming to relieve spinal nerve pressure pain. This procedure is designed to aid patients suffering from chronic pain due to spinal stenosis and related conditions.
Our procedure uses the Vertiflex technique, lifting the space where the lumbar vertebrae are narrowing or bulging (often resulting from spinal stenosis). This process is done under a live X-ray as guidance, placing a small device that opens up the pressure area.
TPC Sacral Fuse
TPC Sacral Fuse provides stability to the joints of patients with sacroiliac joint dysfunction. This condition can cause pain with too little or too much joint movement.
Under live X-ray guidance, a small device is placed into the sacroiliac joint, fusing the joint. Fusing the joint creates better stability, targeting pain caused by movement and instability.
TPC Peripheral Nerve Stimulation
TPC Peripheral Nerve Stimulation offers pain relief to patients suffering from peripheral neuropathy and related conditions. A small electrical wire is surgically implanted along the damaged nerves and delivers rapid electrical pulses. These pulses feel like mild tingles, called paresthesias, and help to minimize pain.
TPC Spine Decompress
TPC Spine Decompress offers a minimally invasive method of pain relief for patients with spinal stenosis. In this treatment procedure, a small trocar needle is used to locate where the narrowing is causing the pain is occurring. Following this, we use a small instrument called the rongeur to remove excessive bone or tissue to open the area.
III. Other interventional methods
Mesdagh, et. al., (2023) also list in Table 1 the following interventional methods:
| Interventional treatments | |||
| Photobiomod-ulation | Localized neuropathic pain | ||
| Neuromodula-tion | 1. Spinal cord stimulation, dorsal root ganglion stimulation 2.Neuraxial drug delivery (morphine, ziconotide, local anaesthetic, baclofen, clinidine, ketamine 3. Percutaneous neurolysis (cryoanalgesia, thermal neurotomy, pulsed radiofrquency) | 1. Neuropathic pain 2.. Refractory pain, opioids intolerance, widespread bone metastases, specific location (i.e., pancreatic cancer.) 3. Neuropathic refractory pain – Breast, upper limb, or posterior cervical spine cancer pain – Abdominal and epigastric pain -Pelvic cancer pain -Lower rectal and perianal burns | |
| Cordotomy | Severe nociceptive or neuropathic pain in short term survival patients | ||
| Percutaneous ablation of metastasis | Radiofre-quency, cryotherapy | Metastatic bone lesions, usually for people with short life expectancy | |
| Vertebroplasty and kyphoplasty | Vertebral instability and spinal cord compression consecutive to fracture | ||
| Botulinum toxin | Chronic pain |
IV. Complementary approaches
In the last section of Table 1, Mesdagh, et. al., (2023) list the following complementary approaches to managing chronic pain:
| Integrative medicine | |||
| Hypnosis | Chronic pain | ||
| Yoga, Tai Chi and Qi Gong | Aromatase inhibitor-related joint pain, chronic pain | ||
| Mindfulness and meditation | Cancer-related symptoms | ||
| Cognitive behavioural strategies | Chronic pain | ||
| Music therapy | Chronic pain | ||
| Acupuncture | Chronic pain | ||
| Massage therapy | Chronic pain | ||
| Spiritual and religious interventions | |||
| Virtual reality | Under research |
I would like to add to the above list the use of transcutaneous electronic nerve stimulation (TENS), which involves the use of a device which delivers recurrent stimulation to neurons via electrodes placed on the skin. The patient is able to control the frequency and duration of treatment.

IVa- Complementary approaches: the psychosomatic component – a case history
In October, 2023, I began doing volunteer work as a stockboy in a local market, opening boxes, applying price stickers on boxes, bottles, and packages, and then placing these boxes, bottles and packages onto the appropriate shelves. I kept doing that until late March 2024, when the back pain I was experiencing was significant enough that I had to stop. I went to a rheumatologist in April 2024, who diagnosed me with DISH in my sacroiliac joint:
- Diffuse = spread out, not confined to a single location
- Idiopathic = with a cause that is not known
- Skeletal = having to do with the skeleton
- Hyperostosis = too much growth of bony tissue
This type of condition can be seen in the following X-ray image from Roentgen Ray Reader, https://roentgenrayreader.blogspot.com/2012/02/diffuse-idiopathic-skeletal_10.html :

So I had a diagnosis, but what was troubling me is why, after my cessation of working as a stockboy, was the pain intermittent? There is (permanent) bony tissue being deposited, so why isn’t the pain continuous?
I posed this question to a colleague of mine, who suggested that there is a psychosomatic component to back pain, and in fact, there has been considerable research which shows that at least among men, there is a definite link between stress and back pain.
In 1977, John Sarno, M.D., had an article entitled Psychosomatic Backache in which he states in the abstract that “…the majority of pain syndromes involving the neck, shoulders, and low back are the result of a benign, reversible process in the musculature which is psychosomatic in nature and which has been called tension myositis…[He] believes that the psychosomatic nature of the disorder places it within the purview of the behaviorally oriented specialty of family practice.”
In his article he contrasts the traditional view of neck, shoulder, and low back pain syndromes being manifestations of postural, arthritic and spondylotic abnormalities with the proposition that perhaps 80% of back pain syndromes are due to a benign, reversible, psychosomatic process within the neck and back musculature.
In Sarno’s view, tension myositis comes about most characteristically following minor trauma, sprain, or strain to some segment of back musculature. Regardless of initial mode of onset, if the syndrome persists most low back pain patients will sooner or later experience recurring acute exacerbations, which may eventually lead to debilitating pain.
The following is a list of factors which tend to aggravate a low back pain syndrome:
- Prolonged sitting
- Prolonged standing in one place
- Walking more than 15 or 20 minues
- Bending, lifting, pushing, pulling
- Isometric or isotonic contractions
- Stretching involved muscle
- Cold
The following is a list of factors which generally alleviate low back pain:
- A short walk after sitting
- Lying in a fetal position
- Local heat, hot shower, tub
- Gentle exercise
In Sarno’s clinic, treatment is through a physical therapy program, consisting of a modality to warm the muscle tissue involved(diathermy, mild electrical stimulation, or ultrasound, alone or in combination as appropriate), massage, and an exercise program designed to encourage mobility and strengthen the trunk musculature, particularly the abdominals.
A cautionary tale: The history of OxyContin

A former director of the US Food and Drug Administration (FDA) stated that OxyContin was “the greatest mistake in medical history”. OxyContin’s development, approval and aggressive marketing are considered by many to be the catalyst for the Opioid Crisis, which has resulted in 645,000 deaths between 1999 and 2021 in the United States alone (https://www.ukat.co.uk/blog/substance-abuse/the-tragic-story-of-oxycontin/) .
Opioids, such as morphine, have been used for a very long time to relieve pain. The problem with the use of these opioids was addiction, so the goal has been to develop a drug with a slow-release mechanism that would provide a steady release of the drug over several hours.
Oxycodone was developed early in the 20th century, and had the same addictive properties as other opioids. However, Purdue Pharma, developed a technology called Contin which created a pill that would release oxycodone over 12 hours.
In an earlier blog, https://addictionsandrecoverydotblog.com/2024/03/13/22-from-test-tube-to-pharmacy-shelf-the-regulation-of-drug-development/, I described the lengthy process through which all drugs must be tested and approved. In the case of OxyContin, there were some irregularities in the evaluation process:
- The trials for OxyContin were very short-lived, often lasting just a few weeks. As a result, the possible long-term effects were never assessed;
- Although the trials may have indicated a lower risk of addiction when OxyContin is used correctly, real-world application saw a different story unfold, with misuse and addiction becoming significant problems.
Once Purdue Pharma got OxyContin approved, the company initiated an ambitious and aggressive marking campaign. With a marketing budget exceeding $200 million a year by the late 1990s, OxyContin was marketed as a miracle drug providing 12-hour pain relief with a less than 1% risk of addiction.
From where did Purdue Pharma get the idea that the use of an opioid for pain relief had such a low risk? It came from a letter about opioid treatment in hospitals, published in the New England Journal of Medicine 15 years earlier, in which the authors stated the following:
“Despite widespread use of narcotic drugs in hospitals, the development of addiction is rare in medical patients with no history of addiction.”
The entire letter, shown below, was paramount to Purdue’s marketing claims, and the company trained its sales reps to cite it:
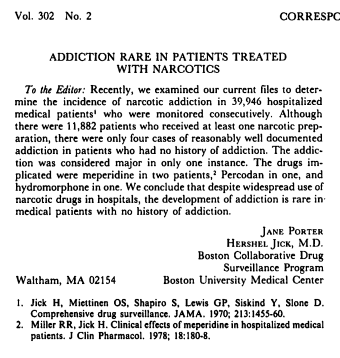
Although the findings of this letter were discredited since then, Purdue used it to target doctors through seminars, paid trips and bonuses. Furthermore, they used various tools to find and target those doctors who were already frequent opioid prescribers throughout the country. Eventually, doctors across the US began prescribing OxyContin to millions of patients who were told there was no risk of ever becoming addicted.
By 2000, sales of OxyContin had grown to $1.1 billion, particularly in rural areas in Appalachia. Although awareness of the problems caused by OxyContin was growing, Purdue continued to offer bonuses to its sales teams, with annual bonuses averaging $71,500 on top of their $55,000 salary. In 2001 alone, Purdue paid $40 million in sales bonuses.
Prior to the marketing of OxyContin, opioids were prescribed only for serious chronic pain, such as cancer-related pain, but Purdue pushed for OxyContin to be used for “non-malignant” pain management, emphasizing that the sense of pain was, in fact, a sixth sense that could be treated.
By the mid-2000s, opioid-related deaths, most of which were linked to OxyContin had reached unprecedented levels. Eventually, in 2007, the company pleaded guilty to misleading the public about OxyContin’s addiction risk and paid a $600 million fine as part of a plea agreement with the U.S. Department of Justice. U.S. Attorney John Brownlee said at the time:
“Purdue acknowledged that it illegally marketed and promoted OxyContin by falsely claiming that OxyContin was less addictive, less subject to abuse and diversion, and less likely to cause withdrawal symptoms than other pain medications – all in an effort to its profits.”
In 2021, Purdue Pharma dissolved, and its assets were used to create a new company dedicated to combating the opioid crisis. The Sackler family was shielded from future opioid lawsuits but had to pay $4.5 billion from their personal fortune over a nine-year period.

P.S.: I’m with ya on this one, bro:
Mesdagh, F.; Steyaert, A.; Lavand’homme, P. (2023). Cancer Pain Management: A Narrative Review of Current Concepts, Strategies, and Techniques. Curr. Oncol. 30:6838-6858. https//doi.org/10.3390/curroncol30070500/
Mills, S.; Torrance, H.; Smith, B.H. (2016). Identification and Management of Chronic Pain in Primary Care: a Review. Curr. Psychiatry Rep. 18:22. DOI 10 10.1007/s11920-015-0659-9.
Sarno, J.E. (1977). Psychosomatic Backache. The Journal of Family Practice. 5(3):353-357.

